A Nurse Is Reviewing the Ecg Rhythm Strip
This post may contain chapter links, which means I get a commission if you determine to buy through my links, at no cost to you. Please read chapter disclosure for more information
Learning how to read an EKG rhythm strip is an essential skill for nurses!
This skill becomes especially handy for nurses on Med-Surg, Telemetry, the Emergency Department, or Disquisitional Care units.
If reading an EKG rhythm strip is new to you – this is the perfect place to start!
What is a Rhythm Strip?
An EKG or ECG stands for Electrocardiography, which is the electrical activeness of the middle traced on paper (or a monitor).
A rhythm strip is at least a 6-2d tracing printed out on graph paper which shows activeness from 1 or two leads.
Leads are "views" of the middle. In that location are 12 leads that are traditionally obtained with a 12-pb EKG, but about portable and bedside monitors but monitor three-v leads at a time.
Luckily – interpreting a single rhythm strip is much easier than a 12-lead EKG. Nearly rhythm strips are interpreted from Lead II every bit this gives a great view of the middle.

The goal of reading an EKG rhythm strip is to determine the rate and rhythm of the patient. This is corking for identifying baseline cardiac rhythm as well as any arrhythmias or ectopy that may occur (like a premature trounce).
A 12-lead EKG also looks at the rate and rhythm, but additionally gives nearly a consummate 360° view of the heart.
This means it can exist used to appraise for things similar cardiac ischemia or infarction, conduction delays, and even enlarged chamber size.
The ECG Rhythm Strip Tracing
As I said earlier – an ECG Rhythm tracing is the electrical activeness of the heart recorded on newspaper or a monitor.
This is traditionally printed out on a 6-second strip. This can brand it easy to determine the rate of an irregular rhythm if it is not given to you lot (count the complexes and multiply past 10).
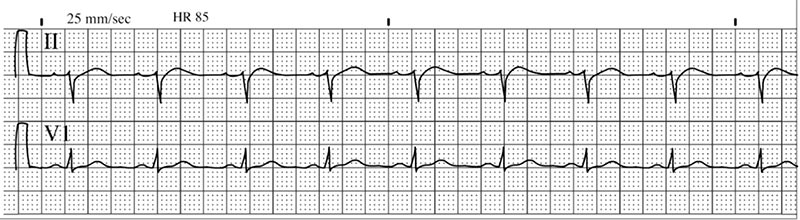
Thick black lines are printed every 3 seconds, then the distance between 3 black lines is equal to 6 seconds.
As you tin can encounter, a printed ECG rhythm strip is comprised of boxes – both pocket-sized boxes and large boxes. 5 small boxes make up one large box.
Each minor box is 1mm broad, signifying 0.04 seconds or twoscore milliseconds (ms).
Each large box is 5 small boxes, signifying 0.20 seconds or 200ms.

This becomes important to remember when determining the charge per unit of regular rhythms. The boxes and lines are also important in recognizing whether a rhythm is regular or irregular.
The PQRST
Okay so that covers the paper, but what nearly the actual tracings? That's where the alphabet comes into play. By alphabet – I hateful PQRST.
An electrical tracing of the heart is made up of waves, lines, complexes, and intervals, and each of these represents specific conduction within the middle. This is the key to interpreting a rhythm strip.
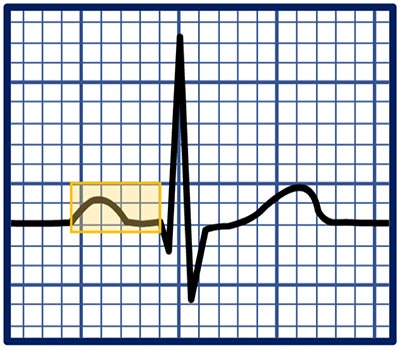
P WAVES
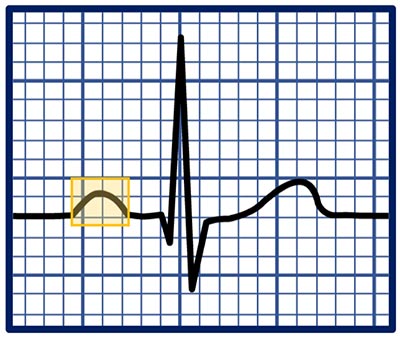 P waves stand for atrial depolarization. This means that the electrical signal that starts in the SA node (the normal pacemaker of the heart) is traveling through both atria (peak chambers of the eye) during the P wave.
P waves stand for atrial depolarization. This means that the electrical signal that starts in the SA node (the normal pacemaker of the heart) is traveling through both atria (peak chambers of the eye) during the P wave.
A P wave should await polish and upright in almost leads including atomic number 82 Two.
The three things y'all'll desire to specifically look for in P waves in a rhythm strip are:
- Are there P waves before each QRS complex?
- Are there any P waves that practice not accept a QRS complex that follows?
- Do all the P waves look the aforementioned / have the aforementioned shape?
Keeping these three questions in mind will help you lot determine where the rhythm originates from (i.e. the sinus node), if in that location are any potential extra beats, or if there could be certain heart blocks present.
An inverted P wave means there is anterograde conduction to the atria (backwards direction). This means the electrical impulse originates from near, at, or below the AV node. Examples of this include Junctional rhythm, certain PACs, and PJCs.
QRS COMPLEXES
 The QRS complex represents ventricular depolarization. This means that the electrical point is traveling through both ventricles (the bottom chambers of the heart). In a healthy heart – this should correlate with the pulse.
The QRS complex represents ventricular depolarization. This means that the electrical point is traveling through both ventricles (the bottom chambers of the heart). In a healthy heart – this should correlate with the pulse.
The QRS complex is actually made up of one-iii waves, the Q wave, the R wave, and the Due south wave. Depending on which lead y'all look at and the specific heart, whatever combination of these waves may be present.
In lead 2, usually all three waves are present. This includes an initial downward deflection (Q moving ridge), an upwards deflection (R wave), followed by a downward deflection (South wave).
The presence of a QRS circuitous indicates that the ventricles are receiving the electrical point. These should follow shortly after a P wave in a sinus rhythm.
 The principal aberration that can occur is a wide QRS complex. This either means that there is aberrant conduction (like a bundle branch block), or that the electrical point starts in either the left or right ventricle (i.due east. a PVC or Ventricular Tachycardia).
The principal aberration that can occur is a wide QRS complex. This either means that there is aberrant conduction (like a bundle branch block), or that the electrical point starts in either the left or right ventricle (i.due east. a PVC or Ventricular Tachycardia).
A packet branch block simply means there is a delay in the conduction tissue transmitting the signal to either the right or left ventricle. If the widened QRS is preceded by a P wave, it is probably a sinus rhythm with a BBB.
If there is no preceding P wave, you lot may accept a PVC or even VTACH if it is sustained.
T WAVES
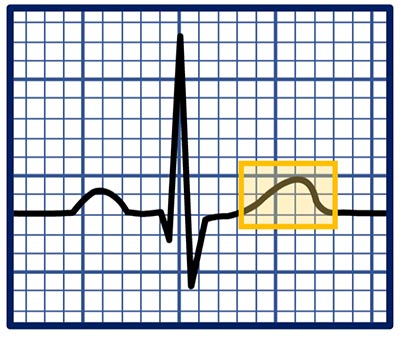 The T moving ridge represents ventricular repolarization. This means that the myocardial cells within the ventricles are recovering and "getting ready for the adjacent beat".
The T moving ridge represents ventricular repolarization. This means that the myocardial cells within the ventricles are recovering and "getting ready for the adjacent beat".
This should be smoothen and upright in most leads, including lead Two.
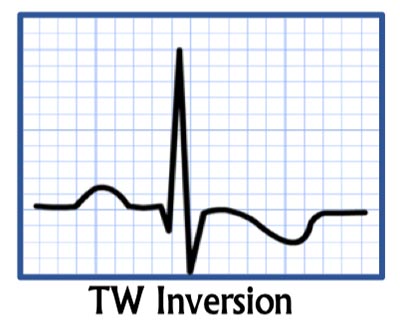 Sometimes, the T wave can be inverted or flipped. This is nonspecific but can bespeak cardiac ischemia or infarction, especially if information technology is in at least 2 face-to-face leads (pertaining to the same anatomical area of the center).
Sometimes, the T wave can be inverted or flipped. This is nonspecific but can bespeak cardiac ischemia or infarction, especially if information technology is in at least 2 face-to-face leads (pertaining to the same anatomical area of the center).
People may have flipped waves in certain leads at baseline afterwards a heart attack, with a bundle branch cake, or with a PVC, VTACH, or ventricular paced rhythms.
Tall or tented T waves are those that are > 1 large box in lead Ii and may exist particularly pointed. This could be normal for the patient, but tin also point hyperkalemia (loftier potassium).
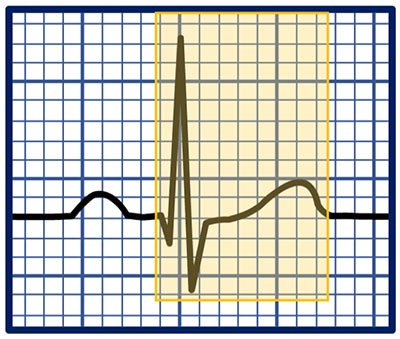
PR INTERVAL
 The PR interval is from the commencement of the P wave to the get-go of the QRS circuitous. This represents the fourth dimension information technology takes for the electrical signal to reach the ventricles from the SA node.
The PR interval is from the commencement of the P wave to the get-go of the QRS circuitous. This represents the fourth dimension information technology takes for the electrical signal to reach the ventricles from the SA node.
This should exist 3-5 minor boxes or 120-200ms. If longer, this is considered a first degree AV cake.
A short PR interval could be from a a PAC, a junctional rhythm (associated with an inverted P wave), or Wolff-Parkinson-White syndrome.
QT INTERVAL
 The QT interval is the time between the start of the QRS complex to the cease of the T wave. This will modify depending on the heart charge per unit, then a QTc (QT corrected) is calculated.
The QT interval is the time between the start of the QRS complex to the cease of the T wave. This will modify depending on the heart charge per unit, then a QTc (QT corrected) is calculated.
This should be 350-440ms in men, and 350-460ms in women. A QT interval >500ms predisposes the patient to deadly ventricular arrhythmias such as Torsades de Pointes.
QT prolongation can be caused by ischemia, electrolyte abnormalities, or from medications such equally psych medications, Zofran, Azithromycin, Cipro, etc.
While you can calculate the QT interval from a single strip, a 12-lead EKG should exist obtained and information technology will be listed on the EKG for you lot. Otherwise, there are online calculators which tin can be used to make up one's mind the corrected QT interval for the heart rate.
Arrhythmias on the ECG Rhythm Strip
An arrhythmia is whatever aberrant rhythm other than normal sinus rhythm – the baseline rhythm of the heart. This can be a benign variant (like sinus arrhythmia), or it could exist mortiferous (like ventricular fibrillation).
In order to know how to read an EKG rhythm strip, you need to showtime exist able to understand what normal sinus rhythm (NSR) looks like.
You should be comparison every rhythm strip to NSR. Recognizing where the rhythm differs from NSR will aid you lot identify the rhythm.
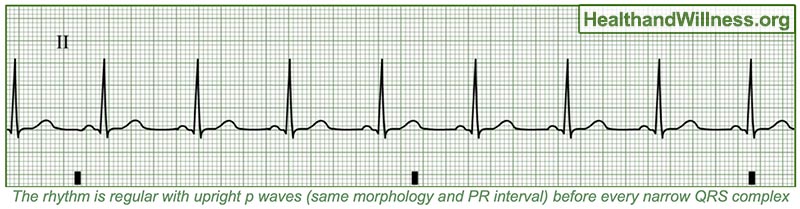
Normal Sinus Rhythm (NSR)
Normal sinus rhythm is the gold standard. This is what a normal functioning centre beat should look like.
The "sinus" in the proper name indicates that the electrical signal is coming from the Sinoatrial node (SA node), the "normal" pacemaker of the middle.
The presence of sinus rhythm means the cardiac conduction system is functioning appropriately (although sure blocks may still be present).
The rate of NSR is 60-100 bpm. Slower is sinus bradycardia, and faster is sinus tachycardia. This just means that the center is performance at altered rates, perchance due to sleep, medications, infection, exercise, etc.
All sinus rhythms should exist regular , meaning each of the QRS complexes are mapping out.
You can do this by measuring the R-R interval between any two beats, and then making sure the R-R interval stays constant throughout the strip. Some people use calipers, but I recommend a proficient quondam-fashioned alcohol pad or piece of paper and a pen.
Additionally, a P moving ridge should precede each QRS complex.
The QRS complex should be narrow unless there is a parcel branch block present.
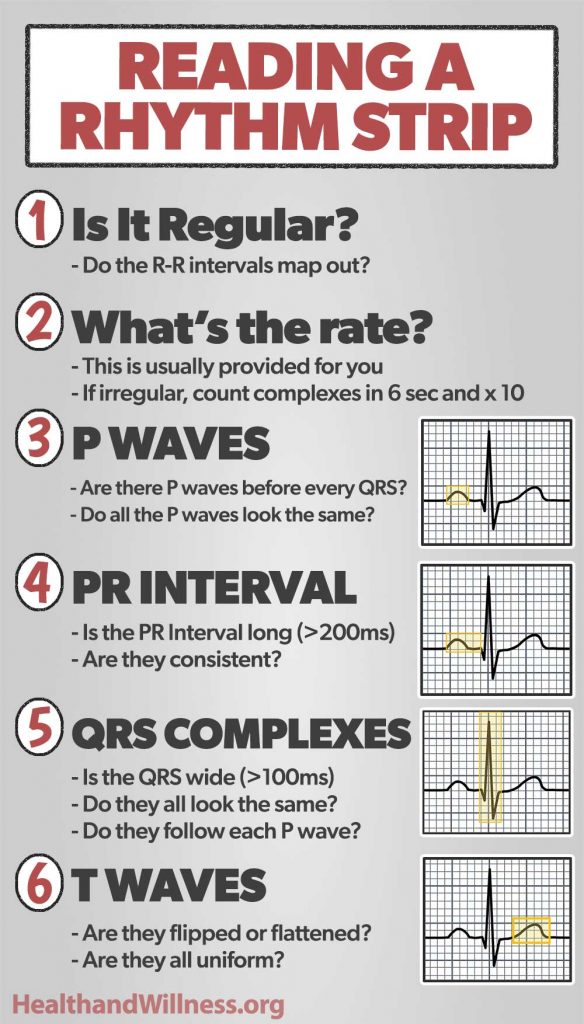
The ECG Rhythm Strip Interpretation
To read an EKG rhythm strip, you should practise and then in a systematic way, so that you don't miss annihilation.
- Is the rhythm regular? Is every R-R interval equal?
- What's the rate? This is usually printed for you
- P wave: Are there P waves before every QRS?
- PR interval: Is it broad >200ms?
- QRS: Is the QRS narrow or wide (>100-120ms)?
- T waves: Are the T waves upright and normal-appearing?
Using this systematic approach should help you lot interpret what each rhythm is. But y'all need to be familiar with about of the arrhythmias out in that location.
Other Sinus Rhythms
Other sinus rhythms are rhythms that may still "normal". I include paced rhythms in this section equally this replaces NSR once a pacemaker is placed.
Sinus Bradycardia (SB)
Sinus bradycardia is the same as NSR, simply the 60 minutes is <60bpm.
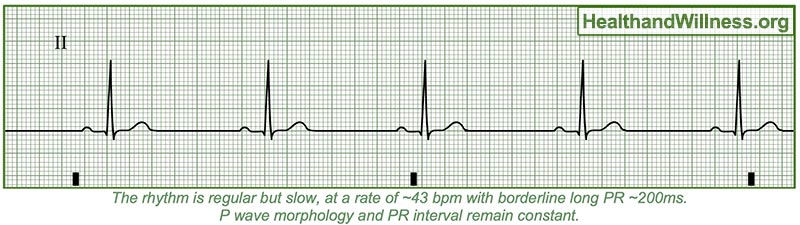
This tin can exist normal for well-conditioned individuals like athletes, tin can be normal if the patient is on a beta-blocker or similar medication, and can also be normal while sleeping.
The most important thing when the patient has SB is
- Is it new or severe (<40bpm or and so)
- Are they symptomatic? (dizziness, lightheadedness, syncope, SOB, breast pain, etc)
Since this is frequently a normal variant – if the patient is asymptomatic there's usually zilch that needs to exist done.
Make sure a boring HR is really SB and not a center block!
Sinus Tachycardia (ST)
Sinus tachycardia is the same every bit NSR, merely the HR is >100bpm and usually <150bpm, at least while at balance.
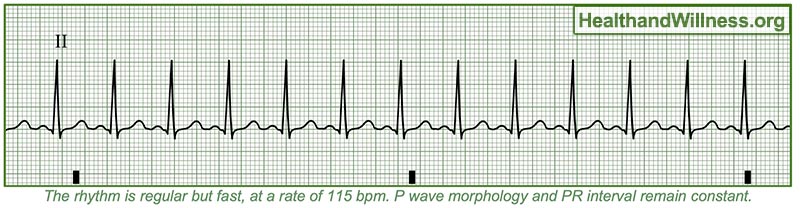
This tin often exist seen with exercise, simply ST at rest often indicates anxiety, sure drugs, sepsis, dehydration, or volume loss. ST is usually a response to an underlying crusade within the torso.
You lot never treat the ST, only rather care for the underlying issue (i.due east. give fluids with volume depletion).
Paced Rhythm
Paced rhythms volition look different depending on the location of the leads. If the lead is in the right atria, the rhythm will announced like NSR merely with a pacer spike before the P moving ridge.
If the lead is in the correct ventricle, it will look like a slow VTACH with a pacer spike before the QRS. There can also exist both of these at the same time.
Some monitors only prove the pacer fasten if you lot plough that function on – if you encounter a very slow VT – ask the patient if they accept a pacemaker and suit the monitors appropriately.
Other Cardiac Arrhythmias
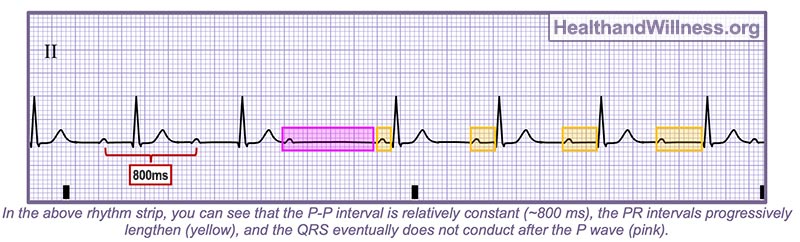
Heart Blocks
Heart blocks are when there is significant delay or blockage in transmitting the point from the atria to the ventricles. This is usually associated with a junctional or ventricular escape rhythm.
First caste AV block is by and large "no big deal" and common in older historic period and with beta-blockers. The PR interval is consistently >200ms.

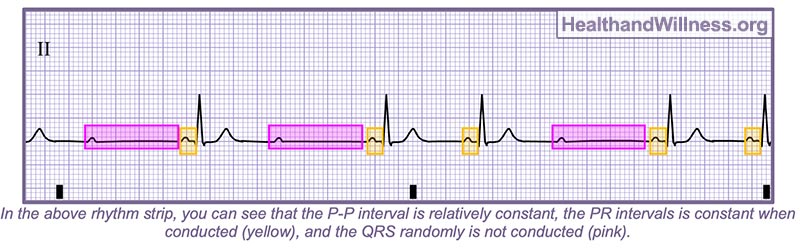
Second degree type 1 AV block or Wenckebach, is when there is a progressive lengthening of the PR interval which eventually leads to a dropped QRS circuitous.
2d degree type 2 AV block or Mobitz II is when there is a consistent PR interval simply QRS complexes are randomly dropped.
Third degree AV block or consummate middle cake is when there is complete dissociation of the atria and the ventricles.

Atrial Fibrillation (AF)
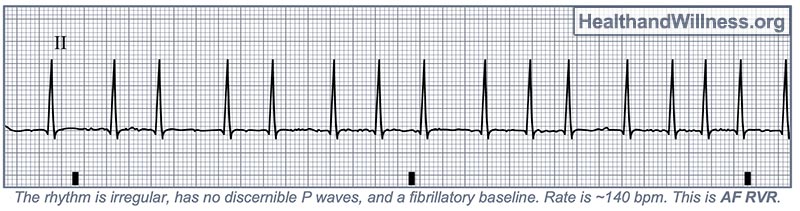
Atrial Fibrillation is a very common type of arrhythmia that you will definitely run into in the hospital. AF could exist new-onset, RVR (rapid ventricular response), could be intermittent (paroxysmal), or chronic/persistent.
AF is an irregularly irregular rhythm , meaning that there is no rhyme or reason for the regularity of each QRS complex.
This is usually from a structurally diseased middle where both atria are quivering speedily, termed fibrillation. This leads to fast ventricular rates (AF RVR), besides as poor blood catamenia through the atria – predisposing the patient to blood clots.
This is why these patients are started on rate-command medications such equally metoprolol or Cardizem, and usually anticoagulants similar heparin, Eliquis, etc.
AF will non have p waves but instead, take a fibrillatory baseline . The QRS complexes will usually exist narrow, and will not map out with each other in any manner.
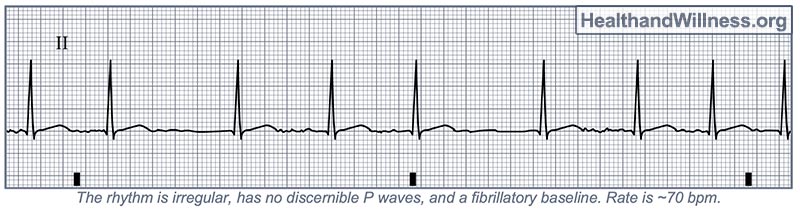
Rates >100bpm are considered AF RVR.
Atrial Flutter
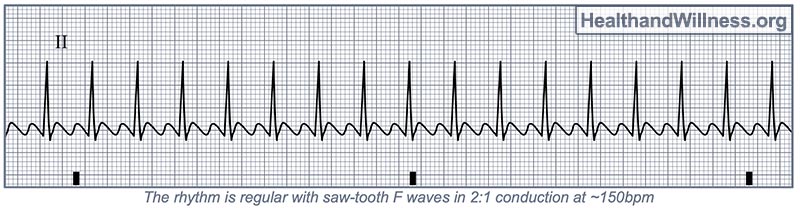
Atrial Flutter (Aflutter) is like to Atrial fibrillation and is treated largely the same.
This is when the atria aren't fibrillating only rather "fluttering". This is commonly from a reentrant loop well-nigh the AV node.
This will ordinarily lead to a conduction ratio of 2:1, and a HR around 150bpm. Conduction ratios can be 3:1 (100bpm), 4:1 (75bpm) and variable likewise.
You will come across saw-molar P waves termed "f waves". Depending on the conduction ratio, yous will encounter 2 (3 or 4) F waves per QRS complex. Aflutter is commonly regular.
Supraventricular Tachycardia (SVT)
Supraventricular Tachycardia is an umbrella term referring to any fast tachycardia that originates above the ventricles. However, in clinical terms, this usually refers to AV Nodal Reentrant Tachycardia (AVNRT).
This occurs when there is an abnormal pathway of conduction tissue near/within the AV node, termed a "reentrant loop".
If a PAC or PVC comes at the wrong fourth dimension, this can send the electrical indicate around and around this loop of conduction tissue, leading to 5ery fast heart rates.
SVT can exist as "tedious" as 140bpm to as fast every bit 220bpm. The faster the heart charge per unit, the more than symptomatic the patient usually is.
In SVT, P waves are unremarkably not present, there is usually ST low, and the rhythm is regular with narrow QRS complexes.
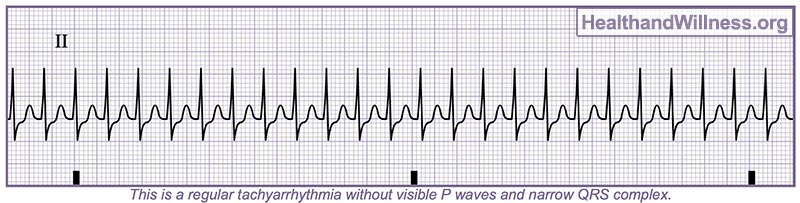
Handling for this involves vagal maneuvers and often adenosine or Cardizem.
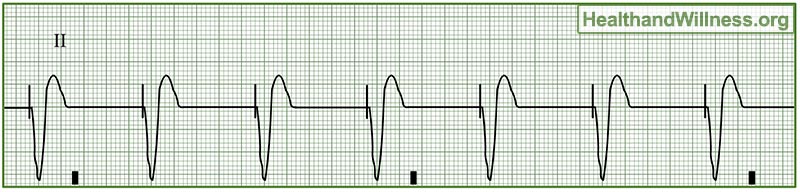
Ventricular Tachycardia (VTACH or VT)
Ventricular Tachycardia is a fast tachyarrhythmia originating within the ventricles. This leads to very fast center rates with or without a perfusing rhythm.
This means the patient may non have a pulse and may be a code blue. Either way, VT is a very serious arrhythmia.
VT is usually acquired past Coronary heart affliction, like a previous or current MI.
The rhythm is regular, and the rate is anywhere from 100-330bpm, and the QRS complex is broad (>140ms).
P waves are normally absent-minded or undetectable, but 60% of cases tin can have AV dissociation nowadays.
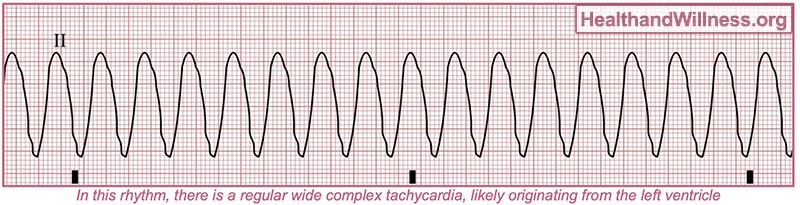
If there is no pulse, you use ACLS cardiac arrest algorithm.
If there is a pulse, you lot utilize the ACLS Adult tachycardia with a pulse algorithm.
Ventricular Fibrillation (VF or VFIB)
Ventricular Fibrillation is a deadly ventricular arrhythmia. There will not be a pulse, and the patient will be coding.
VF is a similar concept as AF, except the ventricles are the ones fibrillating. Coronary artery affliction is again one of the primary causes of VF. Severe electrolyte abnormalities tin can also cause VF.
VF is irregular and has no pattern. There is either coarse or fine fibrillation, eventually degenerating into asystole if non shocked back into a normal rhythm.
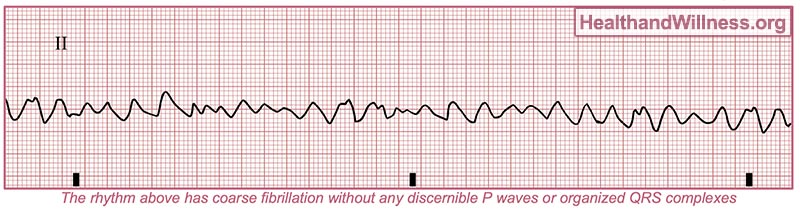
These patients need fast defibrillation, loftier-quality CPR, Epinephrine, antiarrhythmics, etc (Lawmaking blueish algorithm).
Asystole
Asystole is the absenteeism of cardiac activity. This is essentially a straight wavy line but may accept occasional p waves initially. The patient is expressionless. Follow ACLS algorithms as above.

Pulseless Electrical Activity (PEA)
PEA appears like a normal rhythm (Usually NSR or SB), but there is no actual mechanical contraction (no pulse). The patient will be unresponsive, pulseless, and this is a code bluish likewise (follow ACLS).

Desire to learn more?
Hopefully this gave yous a good thought about how to read an EKG rhythm strip. Unfortunately, I couldn't include every single arrhythmia or particular, but this definitely should give you a practiced understanding of the basics!
If y'all want to learn more than, I have a complete video class "ECG Rhythm Chief", made specifically for nurses which goes into so much more depth and item.
With this class yous will be able to:
- Identify all cardiac rhythms within and out
- Understand the pathophysiology of why and how arrhythmias occur
- Learn how to manage arrhythmias like an practiced nurse
- Become proficient with emergency procedures like transcutaneous pacing, defibrillation, synchronized shock, and more!
I likewise include some keen costless bonuses with the grade, including:
- ECG Rhythm Guide eBook (190 pages!)
- Code Cart Med Guide (code cart medication guide)
- Lawmaking STEMI (recognizing STEMI on an EKG)
You tin apply the lawmaking "SPRING2021" for a express fourth dimension 15% discount, exclusive to my readers!
Cheque out more about the course here!
You lot may also like:
- Vagal Maneuvers: How to Stop your Patient's SVT
- xx Tips for New Nurses In the Hospital
- 13 Nursing Myths you lot Probably Roughshod For
- ten Nursing Hacks Every ER Nurse Should Know
Source: https://healthandwillness.org/ekg-rhythm-strip/
0 Response to "A Nurse Is Reviewing the Ecg Rhythm Strip"
Post a Comment